
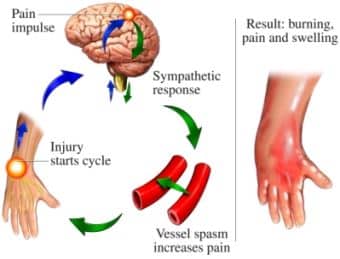
Complex Regional Pain Syndrome (CRPS) Type 1, previously known as Reflex Sympathetic Dystrophy (RSD), is a disorder that may develop as a result of injury, surgery or disease. CRPS consists of unexplained intense pain, altered sensation and reduced motion in the affected body part. The pain, often described as burning, is out of proportion to the injury or stimulus and may gradually increase instead of decrease with time. Other features of CRPS include hypersensitivity to touch, increased sweating, changes in skin color and temperature, and swelling of the affected area.
The exact cause of CRPS is unknown. In some cases the sympathetic nervous system plays an important role in sustaining the pain. The most recent theories suggest that pain receptors in the affected part of the body become responsive (sensitive) to a family of nervous system messengers known as catecholamines (norepinephrine).
Anyone can get CRPS at any age but it is more common in young females. Diagnosis CRPS is diagnosed clinically based on the patient’s symptoms and physical exam findings. There is no specific test for CRPS.
The symptoms of CRPS vary in severity and length. Some experts believe there are stages associated with CRPS, marked by progressive changes in the skin, muscles, joints, ligaments, and bones of the affected area, although this progression has not yet been validated by clinical research studies.
Because there is no cure for CRPS, treatment is aimed at relieving painful symptoms so that people can resume their normal lives.
The following therapies are most often used:
Many different classes of medication are used to treat complex regional pain syndrome, including:
However, no single drug or combination of drugs has produced consistent long-lasting improvement in symptoms.
A gradually increasing physical therapy or exercise program to keep the painful limb or body part moving may help restore some range of motion and function.
CRPS often has profound psychological effects on people and their families. Those with CRPS may suffer from depression, anxiety, or post-traumatic stress disorder, all of which heighten the perception of pain and make rehabilitation efforts more difficult.
Some patients will get significant pain relief from sympathetic nerve blocks. Sympathetic blocks can be done in a variety of ways. One technique involves intravenous administration of phentolamine, a drug that blocks sympathetic receptors. Another technique involves placement of an anesthetic next to the spine to directly block the sympathetic nerves.
The use of surgical sympathectomy, a technique that destroys the nerves involved in complex regional pain syndrome, is controversial. Some experts think it is unwarranted and makes complex regional pain syndrome worse; others report a favorable outcome. Sympathectomy should be used only in patients whose pain is dramatically relieved (although temporarily) by selective sympathetic blocks.
The placement of stimulating electrodes next to the spinal cord provides a pleasant tingling sensation in the painful area. This technique appears to help many patients with their pain. Intrathecal Drug Pumps These devices administer drugs directly to the spinal fluid, so that opioids and local anesthetic agents can be delivered to pain-signaling targets in the spinal cord at doses far lower than those required for oral administration. This technique decreases side effects and increases drug effectiveness.