Scheduling Your Surgery
Once you have decided to proceed with surgery, please contact one of our surgery schedulers to pick a surgery date that is best for you and your family.
Once a surgery date has been picked, our surgery schedulers will work with you to schedule any pre-operative appointments, including your Pre-Anesthesia Evaluation and your first post-operative appointment.
Please be sure that we have updated contact information for you, including a phone number, so that you may be reached prior to surgery. It is very important that we have updated demographic, insurance and primary care physician information to allow for prompt insurance authorization and clear communication.

Important Pre-Surgery Requirements
You are responsible for obtaining surgical clearance from all of your child’s specialists prior to surgery. Some specialists will require an office visit prior to giving surgical clearance so be sure you contact your child’s specialist far enough in advance to allow time for appointment if necessary.
All surgical clearances should be faxed to one our surgical coordinators.
Michelle Davis – Tampa
Diane Bronkema – St. Petersburg
Understanding the Procedure
For a child with a badly curved spine (scoliosis or kyphosis), a spinal fusion is the most common surgery done by our group of highly specialized pediatric spine surgeons. A spinal fusion joins vertebrae together to form a single bone. The goal is to improve the curvature of the spine while maintaining balance and making the spine stable.
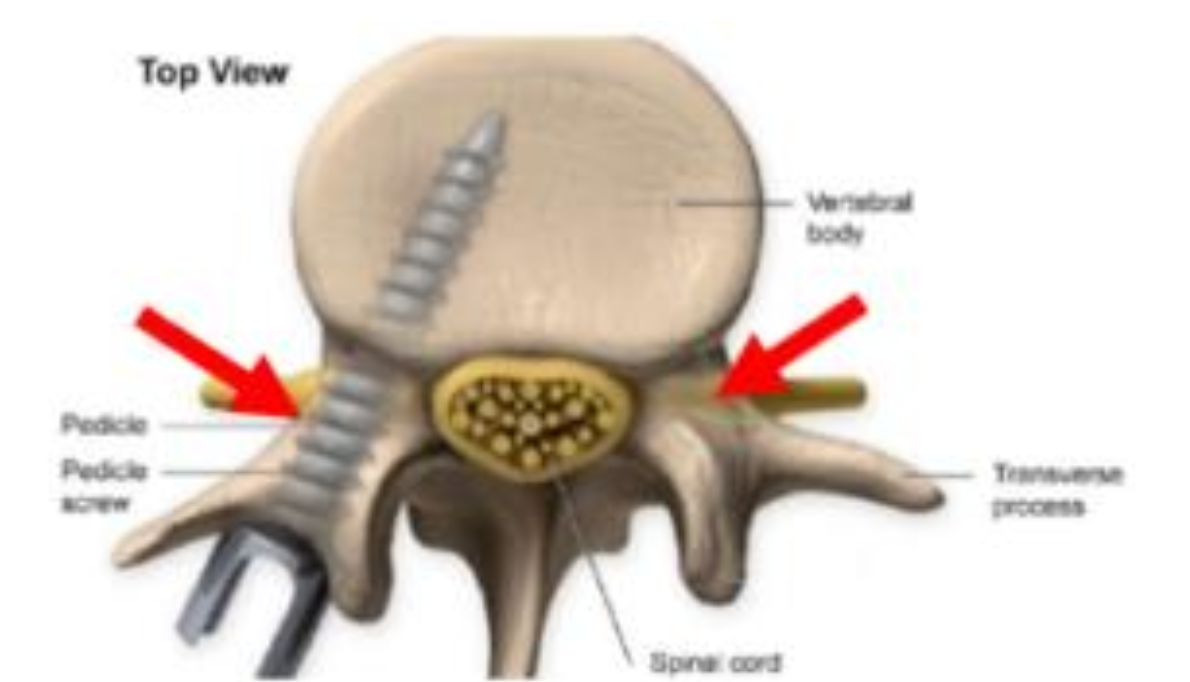
Your spine is made up of 33 vertebrae that stack to form a column. Each vertebra has a hole in the center, forming a hollow channel to house and protect the spinal cord and cerebral (brain) spinal fluid. Extreme caution is taken to protect the spinal cord. We monitor the function of the nerves throughout the procedure.
Once the neuromonitoring sensors are set up and all of the pre-surgery preparation is completed, we begin the surgery.

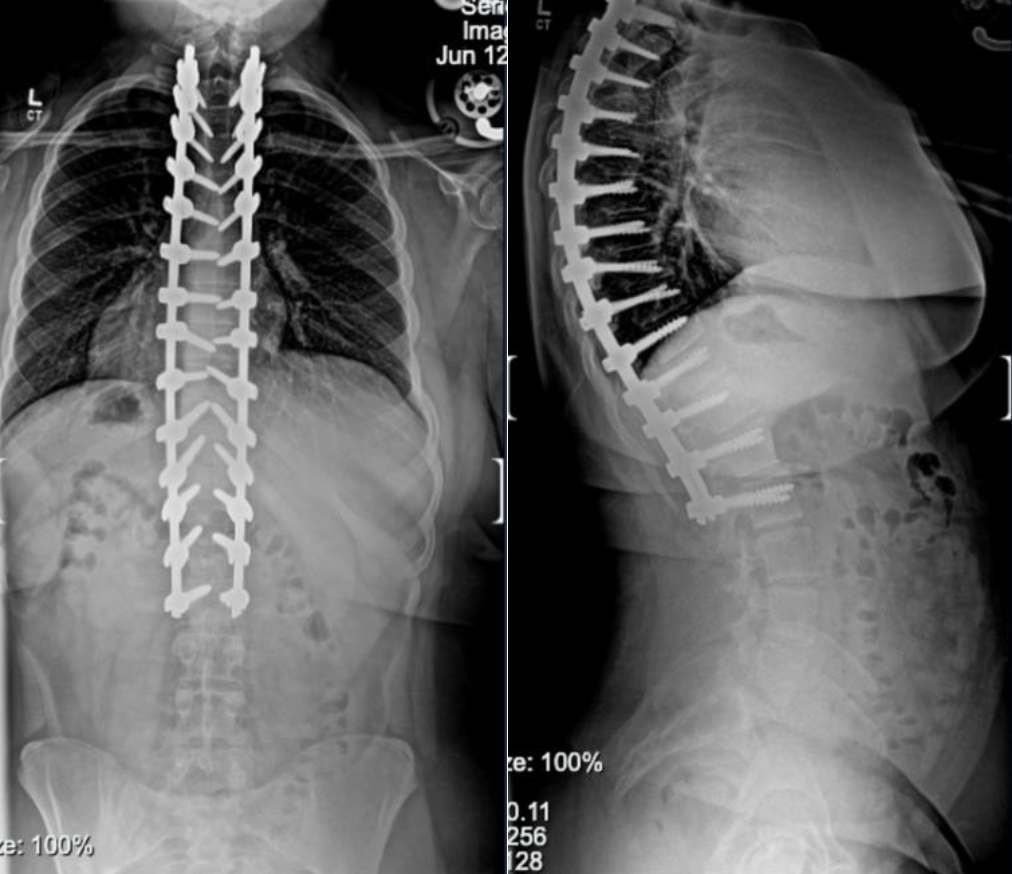
Once we are finished with the surgery, x-rays taken of your spine will show your new alignment as well as the hardware that we used. Below are before and after photos of two of our patients who underwent a posterior spinal fusion, one for scoliosis and one for kyphosis.
Scoliosis


Kyphosis

Potential Concerns to Be Aware Of
Like all surgeries, there will be discomfort after the spinal fusion. To help you get better faster, we use medications to fight the discomfort from every different angle. Walking, having regular bowel movements and eating normally are all crucial to managing your pain.
We do everything we can to control bleeding during the surgery including cleaning and recycling your own blood using a Cell Saver machine. On occasion, when blood counts are too low, it can require a blood transfusion.
You will be given antibiotics during surgery and the first 24 hours after surgery to prevent infection. You will also wash with the Hibiclens Skin Wash two days before surgery to prevent infection. Utilizing clean sleepwear and clean sheets are also important for preventing infections. Despite these actions, infection may still occur. Most infections are treated with antibiotics by mouth. Some severe infections may require admission to the hospital to give antibiotics through an IV and occasionally additional surgeries.

Preparing Early for Surgery
Your child should avoid taking any anti-inflammatory medications such as Motrin, Advil, Aspirin, Ibuprofen, Aleve, etc. However, Tylenol is allowed. It’s crucial to discuss any medications your child may be taking with the surgeon before the surgery.
Ensure we have an updated list of all specialists your child sees, including but not limited to cardiology, pulmonology, neurology/surgery, hematology/oncology, nephrology, etc., to obtain necessary clearance before the surgery date. Failure to obtain surgical clearance may result in surgery being cancelled.
Please inform us if your child has experienced COVID-19, pneumonia, RSV, or MRSA within the last 6 months.
Eat a healthy diet during the period leading up to your surgery. This will help for quicker recovery. Get plenty of exercise so that you are in good shape for surgery.
The Child Life department at Johns Hopkins All Children’s Hospital provides tours and other activities for families seeking more information about their upcoming stay. For further details, please contact them at 727-767-4323.
Housing and Support Services for Families
Families are stronger when they are together. That’s why Johns Hopkins All Children’s Hospital partners with Ronald McDonald House Charities of Tampa Bay to provide the support and resources families need to stay close to their hospitalized child at little to no cost.
Johns Hopkins All Children’s offers families three Ronald McDonald Houses across campus. All locations offer private rooms, snacks, a television and laundry facilities. Some meals are provided. Hospital transport services are also available 24/7 for all locations.
A room request may be made up to 30 days in advance of a hospital stay. All adults 18 years and older must have a background check before arrival and photo ID upon arrival. To request a room at any of the houses, please call 727-767-7694.



Final Preparations Before Surgery
Do not forget to use your preoperative Hibiclens Skin Wash beginning two days before your surgery.
Be sure you have clean sheets for your child’s bed and all areas of the home that they will be recovering in are cleaned. We recommend having a backup set of clean sheets and several pairs of clean sleepwear ready for when your child comes home from the hospital.
Your child will have a pre-anesthesia evaluation at the Johns Hopkins All Children’s Hospital Center for Peri-Operative Optimization (CPO) clinic. See below to learn what that entails:
Steps for Proper Use
Using the Preoperative Hibiclens Skin Wash is a very important step in our effort to prevent surgical infections. You will be provided with a bottle of Hibiclens Skin Wash at your pre-operative appointment in our office. The following instructions should be followed two days before surgery and the night before surgery.
Your child should shower the way they normally do using the Hibiclens Skin Wash instead of their regular soap. Wash especially well from the nape of the neck all the way down to the buttocks.
Do NOT use any lotions, make-up, powders, deodorants or creams. These can interfere with the antiseptic wash and make it difficult for adhesives to stick on the day of surgery.
Dress in clean sleepwear.
Sleep with clean sheets on their bed.
Coverage and Payment Details
It is the parent/legal guardian’s responsibility to make sure we have updated insurance coverage and contact information on each parent or guardian. Please call us if there is any change in the insurance or phone number to reach the patient’s family.
Your insurance coverage will be verified prior to surgery to assess benefits, deductibles, co-insurance, and out-of-pocket expenses, and to initiate authorization. If you have any inquiries regarding your insurance or coverage, please contact the Johns Hopkins All Children’s Financial Clearance department at 727-767-3030.
A surgery deposit may be required before the surgery based on your current insurance benefits. For any inquiries regarding the cost of your child’s surgery, please contact our Financial Estimates department at 727-568-6934.
Please notify your surgeon’s office immediately if there have been any changes to your insurance since your last visit.

Helping You Through the Big Day
We encourage you to only bring essential items the morning of surgery, including:
Wear loose, comfortable clothing. All jewelry must be removed before surgery. This includes: rings, earrings, watches, necklaces, and any other body piercings. Do not use lotions, oils, or perfumes after bathing. Do not apply makeup.
To ensure a smooth check in process, please arrive promptly at the time you were advised of either in your pre-anesthesia evaluation or in your phone call the day prior to surgery.
Your surgery will be performed at Johns Hopkins All Children’s Hospital, located at 501 6th Ave South, St. Petersburg, 33701. Complimentary parking is available in the ACH parking garage adjacent to the Outpatient Care Center.
A bridge on the 2nd floor of the parking garage connects to the Outpatient Care Center and, subsequently, to the 2nd floor of Johns Hopkins All Children’s Hospital. Follow this bridge to reach the hospital.
As you cross the bridge and enter the hospital, you will pass a hallway on your left and then the first lobby/door on your left leads to the Surgical Pre-Registration area. This lobby is marked “H250 Surgical Services”. This is where you will sign in and commence your day with our surgery staff. After signing in, our team will escort you to the Pre-Op Unit.
During Your Child’s Hospital Stay
Your surgery day is here! This day can be filled with emotion and it is completely normal to feel nervous. This section will walk you through exactly what will happen on the day of surgery and throughout your hospital stay.
In addition to the nursing staff on the unit, the Pediatric Orthopaedic surgery team will care for your child. This team is led by your surgeon and includes physician assistants and resident physicians. The physician assistants and residents report directly to your surgeon, who is the one overseeing all of your child’s care. Our service is on call at the hospital 24 hours a day so we are very easily reached if there are any problems or concerns.
We work very closely with the other departments assisting with your child’s care such as Pain Management and Physical Therapy. We all communicate constantly so we are all on the same page when it comes to your child’s recovery.
Your child’s pain will be assessed regularly on a scale from 0 to 10. Pain assessment is necessary to guide your child’s pain relief. It is essential that they are able to take deep breaths, cough, and move. Prevention or early treatment of mild discomfort is far more effective than trying to treat severe pain. Therefore, we have devised a specialized regimen to stay ahead of their discomfort while limiting the use of narcotics.
We utilize a combination of muscle relaxers, anti-inflammatories, and analgesics (pain relievers) to address their discomfort from all angles. If they need additional pain relief, they will have “as needed” medications available through their IV or by mouth—all you need to do is ask their nurse.
The Pain Management team will work with your child daily to adjust doses or swap medications to find the right combination for their comfort. The medications they receive in the hospital will be the same ones prescribed to take home.
Getting Ready to Go Home
Your child’s care team will determine when your child is ready to go home, or be discharged. Typically, they will be discharged from the hospital 1–2 days after surgery. However, their discharge date will depend on their progress throughout their hospital stay.
In order to go home, your child must achieve the following:
We will prescribe your child several medications for them to take at home to keep their pain under control. These will be the same medications they were taking while in the hospital.
A parent or legal guardian will need to be present to take your child home if they are under the age of 18. If your child is over 18, they will need to arrange for someone to accompany them home. They will not be released without someone present.
When your child is leaving the hospital, you will receive an After Visit Summary (AVS). This document includes information about your child’s surgery, incision care, pain management, activity level, diet, home care, and other important instructions.
Call your surgeon’s office anytime if you are worried about your child’s recovery. During regular office hours (9:00 a.m. – 5:00 p.m.), call your surgeon’s office directly. After hours, our main office number will connect you with an answering service, who will then connect you with the orthopaedic PA or resident on call.
Call your surgeon’s office immediately if:
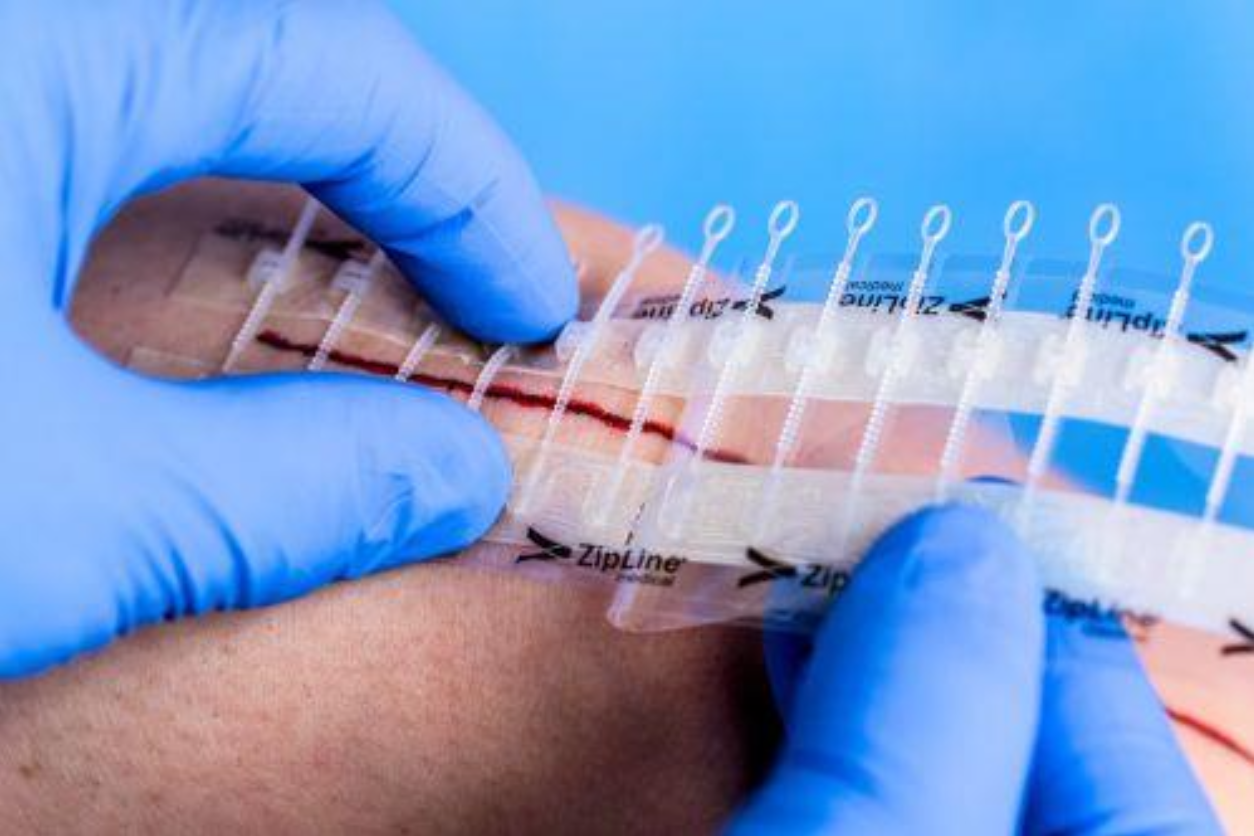
After surgery, your child will have a bandage in place over their incision called Aquacel Ag.
Ten days after your child is discharged, you may remove the Aquacel Ag dressing and ZipLine dressing at home.
You should protect the incision from the sun for the first year after surgery. We recommend using sunscreen with SPF 45 or higher or UV-protective clothing to cover the incision. The more tanned or sunburned the scar becomes, the less likely it is to return to a normal skin tone. Do not apply any creams, lotions, or oils until cleared by your surgeon.
Once cleared by your surgeon, your child may use topical creams on their incision if desired. We recommend using silicone scar bandages to help the scar heal. These can help collagen fibers realign more effectively and are available online. One brand we often use is Nuvadermis.
It is very normal for the sensation around your child’s incision to be decreased or overly sensitive after surgery. This may include numbness, hypersensitivity, or reduced sensation. These changes can be limited to the incision area or extend across a larger portion of the back. Sensations usually improve gradually over the first few months but may take up to two years. Most patients experience mild residual numbness or decreased sensation directly over the incision that may never fully resolve.



It is very important that your child follows all of the activity restrictions that were given to you. Doing too much too quickly can cause problems such as their incision reopening or their hardware breaking, both of which could require a second surgery. Below is a general list of when your child may begin doing certain activities. Do not resume any of these activities until their surgeon has cleared them. If you have questions about any specific activities, please ask your surgeon.
Following surgery, your child’s first post-op appointment will be 2–3 weeks after the surgery date. This appointment should already be scheduled prior to your surgery day.
After that, your child will have appointments at the following intervals:
After the 2-year post-op appointment, no further appointments will need to be scheduled. We will always be happy to see your child in the office for any problems, concerns, or questions.
People have a variety of emotions when facing a major surgery. This is true for both parents and the child having surgery. It is good to look to others for support. Oftentimes family, friends, and people from church will offer to help when they know a loved one is going through a major event. Think of ways you can take them up on that offer to help, such as preparing meals, staying at your home with the other children or pets, or coming to your home to stay with your child while you rest or run errands. Families cope in different ways—time with family and friends, time alone, humor, prayer, communion with nature, meditation, journaling, art, and music.
Some patients and parents find it helpful to connect with another family who has been through the same surgery. We have a list of patients and their families who have gone through spinal fusion surgery and have offered to speak with others about their experience. If you would like to speak with any patients or their families, please notify our office and we will be happy to provide you with contact information.
If you would like to volunteer to share your experience after surgery, please let one of our surgical coordinators know so they can add you to the list.
Typical Recovery Experiences
As your child is recovering at home, we strongly recommend that they take all of their prescribed medications as scheduled instead of waiting for discomfort to return before taking the next dose. When taken on schedule, medications help your child “stay ahead of the pain.” It is much harder to control discomfort once they are already in pain and trying to catch up. As their discomfort improves over the first week or two, they may gradually begin increasing the time between doses.
Note: Please remember that your child just had major spine surgery. While they may not like the idea of taking narcotics and muscle relaxers, these medications are integral to keeping them comfortable during the first week or two of recovery. If they opt not to take them and their discomfort becomes too severe, it will take time to get their pain back under control.
Why is my child having pain in their neck and shoulders?
It is common to experience some discomfort in the neck and shoulders after surgery. The spine is now in a position it is not used to, and the muscles need to adjust to this new alignment. This can lead to muscle pain in the back, neck, and shoulders. Your child should continue with their prescribed pain medications. Once the incision is healed, heat and light massage may also help with neck and shoulder discomfort.
Why does my child have pain or tingling in their thighs?
Some patients report numbness, tingling, or a “burning” pain in the front of their thighs after surgery. This is due to compression on the femoral cutaneous nerve and can be a common side effect. Do not worry—this is temporary and will improve on its own with time. It is not associated with muscle weakness or numbness anywhere else in the legs. However, if your child experiences muscle weakness or numbness in any other part of their legs, ple
It can be normal to have a small amount of drainage from your child’s incision after they go home. You may notice this drainage on the dressing. However, if there is so much drainage that it seeps through the sides of the dressing or drips from the bottom, please contact our office right away.
If the drainage or the incision begins to cause increased pain or develops a foul odor, contact our office immediately. If your child develops redness or the wound begins to open, please take a picture and email it to our nursing staff through the patient portal. Please see page 27 for their contact information.
For instructions on your post-op dressing, please refer to page 19.
After surgery, your child may become constipated for a number of reasons:
If this should happen, here are some solutions to help:
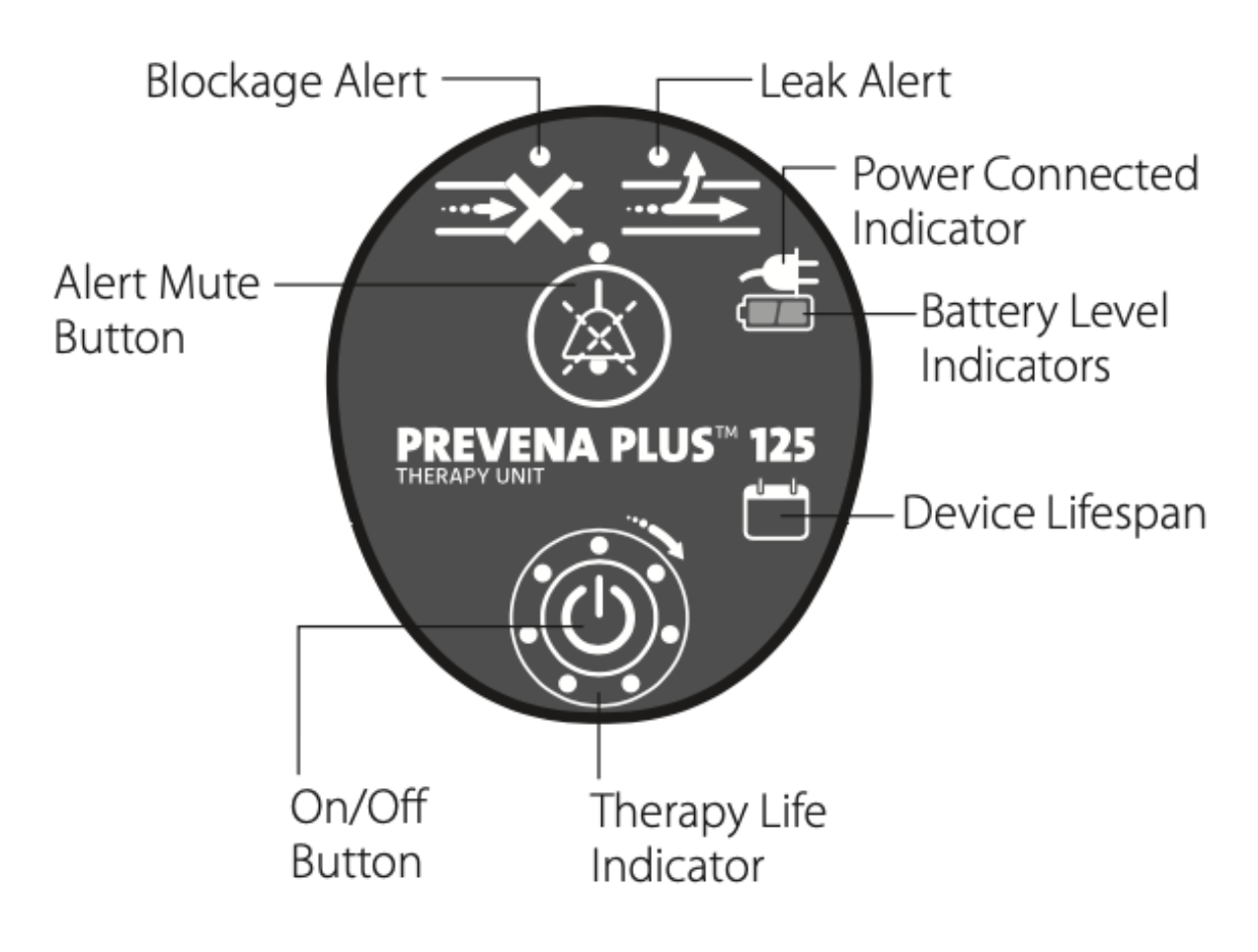
Some patients are discharged from the hospital with a portable wound vac. A wound vac uses Negative Pressure Wound Therapy to help hold the edges of the incision together and improve wound healing.
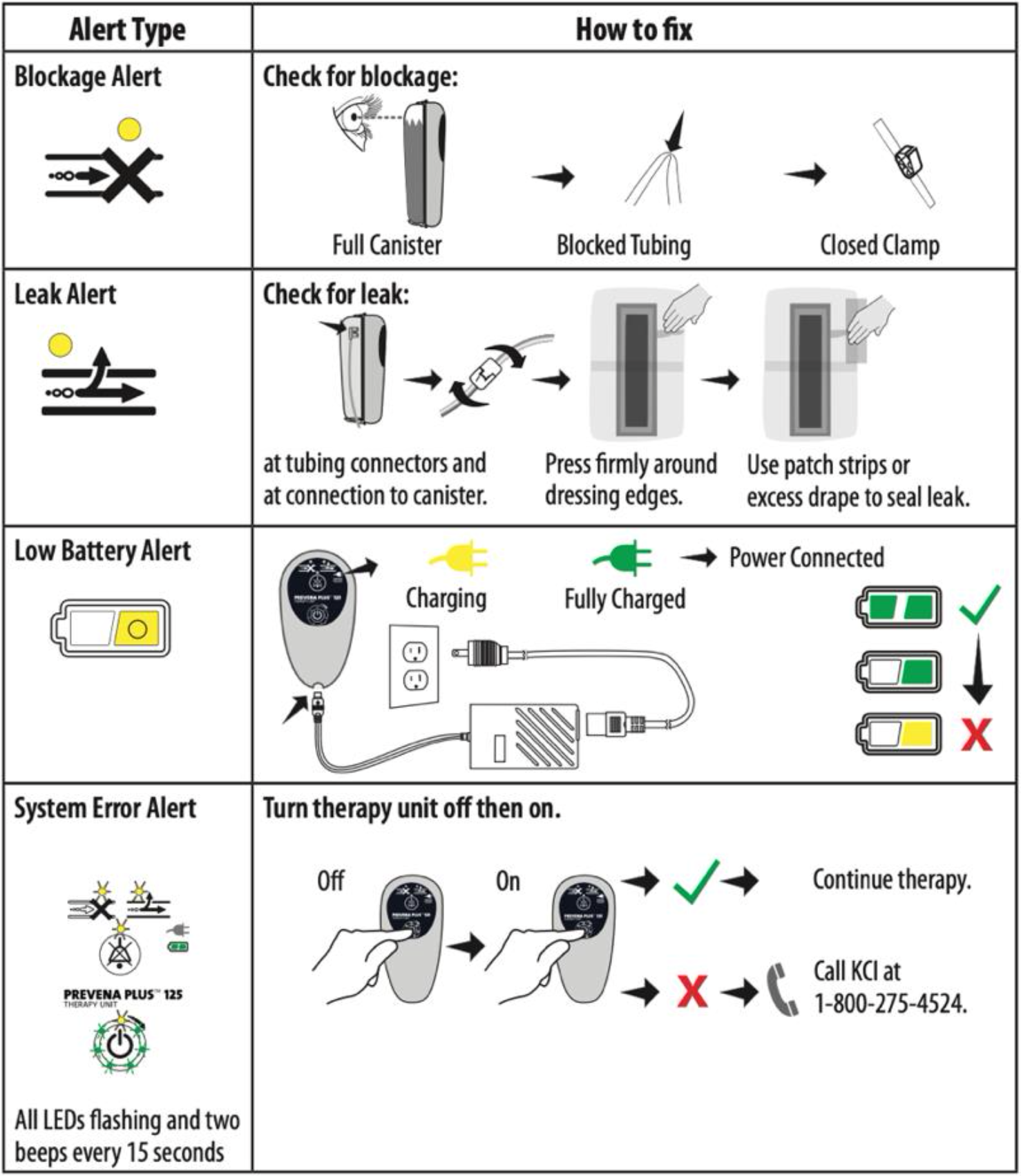
The unit has several indicator lights on the front that can alert you if there is a problem. There will typically be a beeping sound associated with one of the indicator lights turning on. The image to the right demonstrates what each indicator light means.
There are several simple things you can do at home to troubleshoot any problems you may have with your child’s wound vac.
If there is a block: Check that the tubing is not kinked and that the clamp is open. You may also get this warning if the canister is full. If the canister is full or almost full, please contact our office right away.
If there is a leak: Check that the tubing is properly plugged in. Examine the dressing for any edges that may have peeled back or any places where air may be leaking out. If the dressing is leaking air, you can reinforce any areas of leak with the extra dressings you were provided at discharge.
Some Helpful Answers
We recommend that your child avoid driving until 6 weeks after surgery. Not only do they need to be off of all narcotics and muscle relaxers, but they need to have full, pain free range of motion of their back and neck to safely be able to drive. Additionally, their reaction time can be slowed after surgery and they need to allow their body enough time to regain their reaction time.
It is safe for you to travel as soon as you feel comfortable doing so. However, sitting for longer periods of time, particularly in a car or uncomfortable plane seat, can be painful. We recommend walking the aisles of the plane frequently and plan for frequent stops to stretch your legs if driving.
Typically, the hardware used in your child’s surgery will not set off metal detectors. They do not need to carry a card stating that they have surgical implants.
No. Most people feel back to normal after 6 weeks and gradually build their strength back as they slowly begin returning back to normal activities.
The hardware used in your child’s surgery is safe for MRI machines. Be sure to notify any provider who may order them an MRI in the future though as a special type of MRI may need to be ordered to prevent artifact (distortions of the image due to the metal implant) that may affect the accuracy of their MRI.
Up to two adults may stay overnight in the hospital room with the patient. You will have a private room in the hospital with a couch and a cot can be brought in by request. Any visitors must check-in at the main registration desk of the hospital.
Help When You Need It
Michelle and Diane will be your point of contact until the time of your surgery.



