Adolescent hip dysplasia is a condition in which the hip joint has not developed normally. In individuals with hip dysplasia, the acetabulum or hip socket does not develop fully, making it too shallow to contain and support the femoral head connected to the upper leg (see Figures 1 and 2 below).
This causes excessive stress on the socket which can lead to premature degeneration and arthritis over time. If your child mentions hip or groin pain, it may be an early sign of hip dysplasia.


Hip dysplasia can be diagnosed with x-rays and MRI. These images show the dysplasia and can help your doctor find the damage to the labrum and articular cartilage in the hip. Your doctor will also move your child’s hip in different directions to assess the pain or discomfort he or she is feeling.
It’s not known what causes adolescent hip dysplasia, but it tends to run in families and occurs more often in:
Altered forces on the joint can cause damage and pain in the hip. In most cases, this pain is:
Treatment for adolescent hip dysplasia focuses on delaying or preventing the onset of osteoarthritis while preserving the natural hip joint.
If your child has minimal symptoms and mild dysplasia, we recommend simply monitoring the condition to make sure it does not get worse. Your child will have follow-up visits to monitor the hip for worsening symptoms.
Avoiding activities that cause the pain and discomfort may help to alleviate the symptoms. If the child is overweight, losing weight will also help to reduce pressure on the hip joint.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can help relieve pain and reduce swelling.
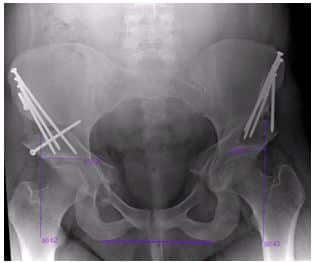
Surgery may be considered if patients with hip dysplasia experience pain and have limited damage to their cartilage. The surgery, called periacetabular osteotomy (PAO) is a procedure which involves a series of cuts to the bone to reorient the acetabulum over the femoral head in order to increase coverage, decrease hip stress, and restore a more normal anatomy. Screws are then placed in the bones to stabilize this position.
This procedure has been shown to have very good results even up to 20-25 years after the procedure (see Figure 2 below).