Children’s Orthopaedics utilizes the most advanced technology available to treat kyphosis, including minimally invasive surgical techniques and computerized intraoperative navigation. Our practice is affiliated with Johns Hopkins All Children’s Hospital and has repeatedly been recognized as Top Ranked Pediatric Orthopaedic Care in Tampa Bay. Our two fellowship–trained spine specialists, Dr. Gregory Hahn and Dr. Ryan Fitzgerald perform over 120 kyphosis procedures each year. Combined, they have over 30 years experience performing kyphosis surgery.
Additionally, our orthopaedic support team consists of knowledgeable professionals who assist our specialists in each step of the procedure, including pediatric nurses and patient care technicians with orthopaedic training, neuro–technologists, fellowship–trained pediatric radiologists, and pediatric anesthesiologists. Kyphosis treatment is often an ongoing process, and our goal is to provide the support and care that your child needs every step of the way.

What You Need to Know
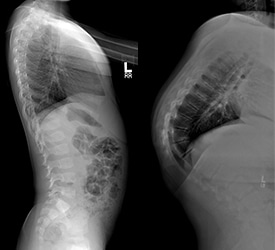
The human spine features several natural curvatures which help our bodies move and remain balanced. The thoracic spine has some degree of a rounded curvature. Kyphosis is an abnormally rounded back. It is a condition that may affect children, teenagers and adults.
The doctor will ask your child to bend forward, to reveal any spinal deformities. This is called the “Adam’s forward bend test.”
What It Means for Your Spine
Understanding your spine and how it works can help you understand kyphosis.
The spine is made up of small bones, called vertebrae, which are stacked on top of one another. Muscles, ligaments, nerves, and intervetrebal disks are additional parts of the spine.


Exploring the Different Types
Congenital Kyphosis occurs when the spinal column does not develop properly while the fetus is still in the womb. The vertebrae do not properly form as they should, or some vertebrae may be fused together. The spinal cord may be at risk of injury with congenital kyphosis. Surgery is frequently necessary.
Postural Kyphosis is the most common type of kyphosis. It becomes noticeable during adolescence, is more common among females than males, and rarely causes pain. It is a non-surgical problem.
Scheuermann’s Kyphosis is the most common type of kyphosis often requiring surgery. Boys are affected more often than are girls. The upper back gradually appears more rounded, and there may be accompanying back pain that worsens during the day and is relieved with rest. Pain, if present, is typically felt at the most curved point of the spine and can be aggravated by activity or prolonged periods of sitting or standing. Low back pain also frequently develops.
The distinguishing factor between postural kyphosis and Scheuermann’s kyphosis on physical examination is rigidity of the spine.
Discover Treatment Options
If your child has kyphosis, it is important to seek treatment. Without treatment, kyphosis can progress, causing functional issues and lower quality of life over time. There are different treatment options available, depending on the severity of your child’s kyphosis. Your physician will suggest the best treatment option for your child. Treatment options can include the following:
Continually observing a small curve to check for progression as the child or adolescent grows.
Bracing may be recommended to prevent the curve from getting worse. Advances in orthotics and prosthetics have led to much more comfortable and lighter weight polypropylene plastic. Unfortunately, to date, no brace has been shown to actually improve kyphosis. That desired outcome is only available via surgical treatment.
The surgical treatment for Scheuermann’s Kyphosis is usually reserved for curves that have progressed beyond 65 degrees. If left untreated, continued progression of these curves may lead to chronic, severe, pain, deformity, psychosocial disability and pulmonary dysfunction. Congenital kyphosis also often requires operative treatment, usually to protect the spinal cord from injury or relieve it from pressure created by the congenital spinal deformity.

Correcting Kyphosis
Pedicle screws are used to anchor the correcting rods to the spine to prevent further movement while the spine is being fused with bone grafts. The screws are used to correct rotation as well as to treat deformity in the coronal and sagittal planes. The pedicle screws can be placed at multiple levels throughout the spine depending on the severity of the curve. The rods are then connected to the pedicle screws.
Growing rods are used to stabilize the spine in very young children with severe kyphosis, sometimes called Early Onset Kyphosis. The rods are placed through the muscles around spine spanning the curve and are usually attached with screws. Growing rods allow for continued, controlled growth of the spine in juvenile patients with kyphosis. The rods are then lengthened on a regular basis, approximately every 6 to 12 months.
Our operating room has been specially–outfitted with advanced imaging technology and specialized instrumentation to accommodate all of our orthopaedic surgical procedures. CT–based, intra-operative image guidance allows the surgeon to navigate the spine using “smart tools.” The data from a CT scan of the spine taken before the operation is used to plan the procedure, including selecting the correct screw size and placement. These images are merged with real–time images of the spine during the procedure so that the surgeon has accurate reference points on where to place fixation devices.
This technology facilitates rapid and accurate placement of pedicle screws—there is virtually no chance of inaccurate placement. It also allows for more precise sizing of the screws within the pedicles and the vertebral body by allowing your surgeon to measure the pedicle and select the correct size. This reduces the chances of loosening or having the screws stick out from the bone.
Dr. Hahn uses this technology very often in kyphosis surgery. Surgeons from around the world visit them at Johns Hopkins All Children’s Hospital to learn about these cutting-edge techniques.
Intra–operative neurophysiological monitoring helps protect your child from neurologic damage like paralysis. The goal of such monitoring is to identify changes in brain, spinal cord, and peripheral nerve function before irreversible changes occur. Motor and sensory monitoring of the spinal cord is conducted with every kyphosis procedure our surgeons perform in order to complete the case safely and efficiently.
Healing After Kyphosis Surgery
After surgery, your child will need to stay in the hospital for about a week. Following discharge from the hospital, your child will need to recover at home for about 3 weeks, on average. If school is in session, you may want to arrange for about 3–6 weeks of homeschooling with your child’s school.
During the recovery period, your child will need to avoid running, bending, and twisting at the waist. Your child must also avoid lifting anything heavier than 5 pounds. Full recovery can take from 6 months to 1 year, as the bones must achieve a solid fusion. After full recovery, your child can resume all normal activities, except for contact sports.
After kyphosis surgery, most patients will be able to function normally at the level they were prior to surgery. In most cases, additional procedures are not needed.

Board Certified Orthopaedic Surgeon

Board Certified Orthopaedic Surgeon